A common experience I remember from my early days as a psychiatrist was the tension I’d feel before seeing a new patient, whether it was a clinic intake, a new admit on the unit, or a consult in the ER. My first thought would be, “Oh, what if I don’t know what to do?” I hadn’t laid eyes on the patient yet or known a lick about them, and already I worried that I would be irrevocably stumped.
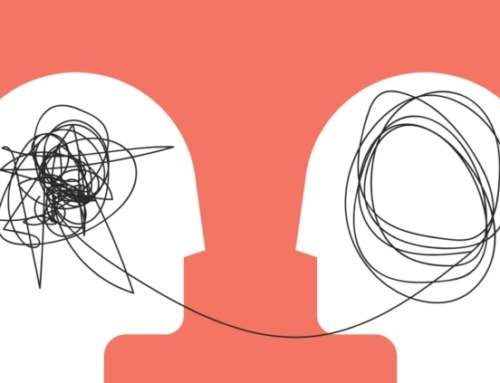
Over the years I learned to trust myself or, more accurately, to trust the patient to “tell” me what their struggle was, and from that to trust that the solution would reveal itself to me. The irony was that the more I rushed and tried to control an assessment, the less opportunity I gave to the patient to “tell” their story and the more elusive the treatment plan became. Patience was needed: more open-ended questions, more listening, longer moments of silence, and greater awareness of subtle and not so subtle behavioral cues.
Twice in the above paragraph I used the word “tell” and placed it in quotes. This is to signify that “tell” is more than verbal communication, especially more than just explicit and well-organized information. After all, patients communicate what ails them not only through report and explanation, but also through demonstration, through behaviors that can include yelling, crying, cajoling, intimidation, seduction, distraction, garbled speech, odd posturing, adventitious movements, clothes grossly inappropriate to the weather, flat facies, suspicion-filled looks, and many, many other such “tells.”
This reminds me of three patients with schizophrenia or schizoaffective disorder each of whom I treated for years. Each had a recurrent “tell” that clued me in to their state of mind better than what they reported to me. When these patients were decompensating, they became paranoid and distrustful of me. This distrust led them to hide their increasing psychosis and to fake-looking good. Of course, after a certain point, they could not keep up appearances or continue keeping their appointments with me. But, of course, I didn’t want to wait to intervene until their psychosis was floridly evident to all. The good news was that each of these three men had a “tell” that their psychosis was resurfacing, and this tell was something they couldn’t hide, or didn’t know how to hide, from me.
The first patient’s “tell” of paranoia was that he walked very close to the wall as I accompanied him from the waiting room to my office. It’s not that he simply avoided walking down the center; rather, he positively hugged the wall on our walk to my office, as if he were a soldier in a battle zone. My second patient’s “tell” was that he sat with his feet not touching the floor of my office. This was a subtle “tell” because my office chairs were the swiveling kind with five splayed legs. Many people sat resting their feet on these legs. He made the “mistake” once of admitting to me that he believed my floor was sending electrical signals through his body to control his mind. This was in response to my asking him once why he had entered my office walking so funny, kind of on his tiptoes. Of course, once he told me his paranoid belief, I remained aware of the sitting-with-feet-off-the-floor “tell” for the next few years that he remained in treatment with me. I probably saved him several hospitalization by intervening earlier than I otherwise would have based on this “tell.” The third patient was the most high functioning of the three and was very good at faking good during the time he spent in my office and waiting room. His “tell” differed from the others. The “tell” in his case was there would be a phone call to the clinic from his father. The first time his father called to share his concerns about his son with me, I didn’t believe him, first, because he wasn’t really clear about what was concerning him about his son’s behavior and, second, because his son looked fine during his visit with me. Of course, I learned within a few days that his father was right, after his son was hospitalized in florid psychosis. After that, I didn’t even need to call the father back – I always did call back, of course – to know that the call meant that his son was decompensating. I learned to stop trusting my “lyin’ eyes” that all was well and instead trust the phone call from father who was more adept at picking up signs of his son’s impending decompensation.
Let me now return to the top: my point today is to trust the problem to reveal its solution. The examples above illustrate how sensitivity to nonverbal cues can lead to a change in treatment plan in cases in which patients are unable or unwilling to report on the nature of their problem. But there are many scenarios that differ dramatically from the above examples that also illustrate how focus on recognizing and understanding the problem leads to its solution. Here’s an example from a very different kind of patient. The patient described below, who I refer to as Daniel, was a never-married man who suffered from chronic dysthymia with intercurrent major depressive episodes. He also spoke of relationship problems, loneliness, and heavy alcohol use which he stopped about two years earlier. Below I recreate part of my conversation with him, after he discussed chronically feeling “miserable.”
I asked Daniel, “Tell me what ‘miserable’ feels like.”
He stared at me without answering, slightly annoyed.
Undeterred, I asked, “One thing I mean by this is what does the physical sensation of feeling miserable feel like?”
This way of putting it seemed to spark understanding in Daniel. He said, “It feels … empty … maybe that’s too strong. It … I mean, I feel “blank or flat…. Or, maybe hollow. Yes, hollow describes it best.”
“And where is this hollow feeling located, in what part of your mind and body?”
“Hmmm. In my chest, like my chest is concave, as if it was scooped out in front… when it’s bad, that feeling is bigger and feels like my entire chest and abdomen are hollowed out.”
“Yes,” I said, “Take a moment now to bring that feeling up … Once you have it, notice what else is going on. What other sensations do you notice? What thoughts, words, or images enter your mind? What emotions come up? Then, think about what this experience reminds you of. A good place to start, although not the only one, is to think about when you first had this hollow feeling in your chest and abdomen.”
Daniel sat silently for what seemed like a long time, 5 minutes I’d guess. By this point in my career, I learned to trust myself to remain silent. It wasn’t easy. It’s not that nothing was happening. Maybe too much was happening, maybe the most that had happened to him in years. The most important thing was for me to avoid disrupting whatever he was remembering, imagining, feeling.
Finally, Daniel said, “Yes, I see. I was able to recollect [He had an academic way of speaking] events from my childhood. I felt lonely much of that time. I didn’t understand other kids and they didn’t understand me. I didn’t have friends. As an only child, I only had my parents. They weren’t bad parents. No abuse or anything like that. But also, not a lot of closeness or even interest in me. They often talked about my grades and how I needed to apply myself…. But that’s different than showing interest in me, in me as a person. It felt like they just needed to have a successful child, someone who would grow up and be as successful as they were. I think I started to have that hollow feeling inside when I would stand there listening to them talk to me about my grades and other things that seemed like markers of success. And when they were done talking, I would just go back to my room and sit on my bed.”
Now, I don’t mean to suggest that the clouds parted and Daniel left my office a changed man. He didn’t. He didn’t come to me for psychotherapy – I managed his antidepressants. But it did change the focus of his therapy with his therapist, he told me. He did gain an opening – identified that crack – into his lifelong unhappiness. I lost track of him later but like to believe that the opening lead eventually to some sort of resolution.
Thanks much for reading.
Dr. Jack
LanguageBrief
Today’s Quotes
“The only normal people are the ones you don’t know very well.”
Alfred Adler“Home is not where you were born; home is where all your attempts to escape cease.”
Naguib Mahfouz“It is easier to act yourself into a new way of feeling than to feel yourself into a new way of acting.”
Harry Stack Sullivan“Life is best organized as a series of daring ventures from a secure base.”
John Bowlby




Leave A Comment