In response to my post from two weeks ago regarding suicide, a colleague wrote me with the following comment and question,
“I’m an early career psychiatrist working with an underserved population. Most of them are chronically sick and with lot of irreversible factors. Appointments are 15 minute med checks. So, two things:
A) How can a time efficient assessment be made every time?
B) How do I do appropriate documentation about it?”
Today I attempt to answer the first question and defer discussion of documentation for a later post. Given how challenging such situations are, as described by our colleague, let me start by approaching this question broadly.
Many of our patients face complex webs of (biopsychosocial) problems. Wherever they look they see problems, ones that are so multiple, far-reaching, and entwined that a way past them seems unattainable. Certainly, persons who are overwhelmed have diminished problem-solving capacity – that’s part and parcel of the overwhelmed state – but their sense of the breadth and depth of their problems also is an accurate reflection of the state of their world.
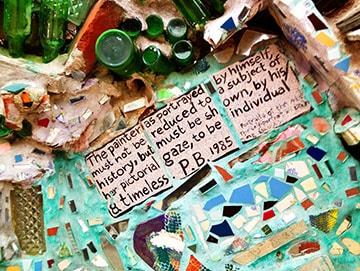
Weekly Photo
Above is a close up of Isaiah Zagar’s “Magic Gardens” mosaic, garden, and art center. It’s located at 1020 South Street, Philadelphia.
Further, it’s also not uncommon for a clinician to fall into a sense of overwhelm when trying to develop a treatment plan for the patient. The clinician can begin to experience their own uncomfortable emotional state of overwhelm, to develop a sense of hopelessness about finding workable solutions, and at times to experience a wish to avoid the patient, a person who triggers such uncomfortable thoughts and feelings in them. Such a clinician attitude is called therapeutic nihilism and is a constant danger all of us clinicians face.
So, with that as background let me suggest a way forward. The first step to finding solutions is completing an assessment, of course. The foundation of learning the scope of the patient’s problems and potential solutions can be laid at the initial evaluation, thus allowing the clinician to effectively and efficiently follow up on the items in the patient’s problem list during, even brief, follow-up sessions. Let me introduce two categories of questions we can (and should) ask our patients during an assessment.
Fact-Based Questions
Our most commonly asked questions focus on the facts of the patient’s life, including their medical and psychiatric symptoms and treatments. Of course, a patient, like anyone else, can be mistaken about some facts. Nonetheless, the goal is to ascertain as many diagnostically- and treatment-relevant facts about the patient as possible. Questions in this category include:
- Have you been in treatment before?
- What symptoms are you having? How’s your appetite, your sleep, your energy level?
- How bad does your depression get?
- Do the voices ever tell you to hurt yourself?
- What medications are you taking?
Questions in this category form the foundation for establishing a diagnosis and treatment plan. But if a clinician asks nothing other than questions from this category they may be doing themselves and their patients a disservice. Regarding the disservice to themselves: the clinician is leaving the entire burden of developing a treatment plan on their own shoulders. Of course, the buck always stops with the physician but that doesn’t mean the patient can’t be a great resource for finding a way out of the mess. And regarding the disservice to the patient: the patient is, in many ways, the expert on their own life and experience. They have much more to offer the treatment planning process than just answering fact-based questions. If you ask a different kind of question, the patient may end up receiving better care. This point now leads us to the next category of questions to ask the patient.
Judgment-Based Questions
It can be incredibly freeing and informative – sometimes eye opening – to ask for the patient’s opinion about some aspect of their condition or treatment. In effect, you are treating them like an expert and asking for their “professional judgment.” Question falling in this category include:
- Out of all the medications you’ve taken which one worked best for you?
- If you were the doctor, what would you recommend to yourself about how to get past this particular problem?
- What do you think went wrong that made you end up getting hospitalized this time?
- What do you think we need to get in place to help you better succeed on the outside?
- Do you notice a pattern in how your depression and suicidal urges start and get stronger?
- If you could change only one thing to feel like life is worth living again, what would that be?
- Many of the problems you told me about cannot be directly fixed by you or by me. What is one thing YOU can do, in your opinion, to make this problem less of a problem?
- If a miracle occurred and all your emotional problems resolved, what would you choose to do with your life?
- Why?
Haha – I end with the question ‘Why?” It’s such as simple question and one that can be used in so many different contexts. I’ve taught over three thousand psychiatrists interviewing skills over the years and, especially among residents, it sometimes seems like there is an implicit rule against asking the patient why they did something or didn’t do something. It almost seems like its cheating to ask the patient to explain their possible motivations. Or perhaps rude somehow.
I’m here to tell you that no such rule exists. And if it did, it would be wrong. We ask ourselves and family and friends “Why?” all the time. Why not do the same with patients? (See how I just asked you a “Why?” question there?)
To return to our colleague’s question about how to conduct a time limited assessment: by asking the patient to share their opinion and recommendations regarding what are the biggest drivers of their suffering and risk, you will be in a better position to decide what are the most important interventions you can deploy to address those priorities.
A person can have a thousand and one problems, but they cannot – and neither can you – resolve all of them – not now and, perhaps, not ever. But rather than getting overwhelmed, focus on the one or two things the patient has told you that could make a noticeable difference. Make a plan and follow up on progress even during the briefest sessions.
Until next time,
Dr. Jack
LanguageBrief
Today’s Quotes
“So many words get lost. They leave the mouth and lose their courage, wandering aimlessly until they are swept into the gutter like dead leaves. On rainy days, you can hear their chorus rushing past: I was a beautiful girl Please don’t go I too believe my body is made of glass-I’ve never loved anyone I think of myself as funny Forgive me….”
– Nicole Krauss, A History of Love“The word ‘listen’ contains the same letters as the word ‘silent’.”
― Alfred Brendel





Leave A Comment