Today I share with you three ideas about suicide and its management. One, we cannot predict suicide. Two, we can manage the risk and decrease the rate of suicide. These two ideas are based on mountains of research, some of which I share with you below.
But notice that these two ideas are in seeming conflict: how can you influence a future event if you cannot predict it? I propose an answer, which is the third idea that I share with you today.
Weekly Photo
Above is another street mural from Chicago, from the La Villita neighborhood, on a building off 26th street.
First, let me expand on the first two ideas. Here is an excerpt from a recently published meta-analysis (by Franklin et al, 2017) that evaluated 50 years of research on suicide risk factors and their ability to predict suicidal thoughts and behaviors [STB]:
“This meta-analysis found that, based on the existing literature, all STB risk (and protective) factors are weak and inaccurate. This general pattern has not changed over the past 50 years and was not meaningfully moderated by study characteristics (e.g., length, sample severity) or type of risk factor (e.g., internalizing psychopathology, prior STBs).”*
Ouch. This important meta-analysis shows us how far in the woods we are. The authors suggest we are in a preparadigmatic stage in our understanding of the causes and moderating factors for suicide and suicide-related symptoms. But life (and death) goes on. We don’t have the luxury of taking a break from treating patients until we gain a better understanding in some future world. Luckily, we don’t have to; here is a list of medications that have been found to decrease suicide:
- Lithium: decreases suicide risk in bipolar disorder and in MDD by 60% compared to placebo
- Clozapine: decreases suicide risk in schizophrenia and schizoaffective disorder
- Antidepressants: decrease suicide risk in depressed patients 75 years of age and older
Now, here is a list of psychosocial interventions that decrease suicide attempts:**
- Cognitive therapy for suicide prevention (CT-SP)
- Cognitive behavioral therapy (CBT)
- Dialectical behavioral therapy (DBT)
- Mentalization-based therapy (MBT)
- Problem-solving therapy (PST)
- Psychodynamic interpersonal therapy (PIT)
- Multi-systemic therapy (MST): in adolescents
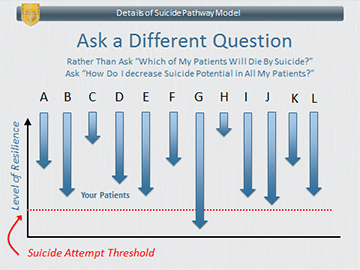
If I’ve been clear in my argument you are probably still thinking, “How can these two ideas both be true? How can we decrease rates of suicide among our patients if we can’t predict who will do it and when they’ll do it?” I’m about to answer this question, but first let me show you the following slide I made for my (free) suicide management course, which provides a foundation to getting to my answer.
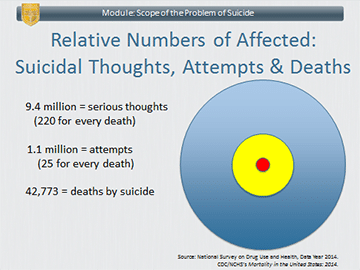
These three concentric circles are proportional in their surface areas to the number of persons in 2014 who suffered from three different suicide-related outcomes. The people in epidemiologic surveys who endorsed having “serious suicidal thoughts” are represented by the large blue circle; the ones who in those same surveys who endorsed making suicide attempts are represented by the medium yellow circle; and the ones who actually died by suicide are represented by the smallest red circle. (Note that this is a simplified illustration because these three circles are not perfectly concentric, that is, some people who die by suicide may have been outside of the yellow circle or even the blue circle.)
This is what I mean by “suicide is a problem for the living.” It means that the great majority of people who suffer with suicide-related symptoms will never die by suicide. It also means, as I discuss below, that even the ones who do die by suicide, we do not know ahead of time, who they will be. I will go so far as to say, that even they, the people who will proceed to die by suicide, don’t know much ahead of time that they are the ones who will die by suicide!
These three circles highlight that there is a high base rate in the population of suicidal thoughts and behaviors, along with a low base-rate of death by suicide. In statistical terms, in such a situation, the presence of various risk factors has low predictive value for the outcome of suicide, irrespective of the sensitivity and specificity of the risk assessment instrument used to assess for those risk factors.
Of course, the circles represent findings across the entire population. The risk of suicide is higher among persons with psychiatric disorders who may be in treatment with us. Their rate of suicide is increased by somewhere between 5-20 fold, depending on the type of disorder and its severity. Thus, having a psychiatric disorder confers a high relative risk for death by suicide, but still results in a rather low absolute risk: On average only about one in 750 persons in our care will die by suicide each year (as compared to one in 7,500 in the general population).
OK. With that as context, this is my way of thinking about suicide. Suicide risk is elevated across almost all psychiatric disorders. Thus, nearly all of our patients are at increased risk for suicide, although their relative risk, even among very sick patients, is low. Further, we cannot know which persons in our care will proceed to die by suicide. For every 220 who endorse serious suicide thoughts, only one will proceed to die by suicide. And even that is not accurate since, as I pointed out, that one person may not have endorsed having suicidal thoughts and thus, would be outside the large blue circle.
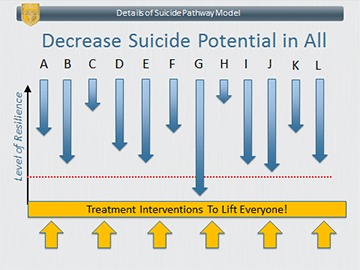
So, this is what I ask you to consider: treat all your patients as being at risk of suicide and intervene with ALL your patients to decrease their risk of suicide. Is this realistic? After all, isn’t it “overkill” to provide suicide-decreasing interventions to every patient even when their risk is very small? It could be, but here is the crux of my recommendation: suicide-decreasing interventions are just GOOD interventions for everyone. Suicide is related to intense suffering. Most people intensely suffering will not die by suicide. If you intervene to decrease suffering (and provide alternative coping strategies) then you are helping ALL your patients. There is no “wasted effort” providing suicide-decreasing interventions to all patients, because all patients will benefit from it. An analogy is providing nutritional counseling to all patients in an internist’s office when only some may have high cholesterol or high blood pressure. Even if they didn’t have tests for assessing cholesterol and blood pressure and had to provide it to everyone, wouldn’t nearly all patients benefit from such counseling in one way or another?
Here are a couple of slides that illustrate my point. (Each arrow represents an individual patient. Down represents falling into suicidal crisis and up represents maintaining resilience against suicide.)
In a future post, I’ll present some interventions to help you “lift” everyone up from suicide risk and how to do so with a minimum of time and fuss.
Until next time,
Dr. Jack
LanguageBrief
Today’s Quotes
“Ask not what disease the person has, but rather what person the disease has.”
– William Osler“If [suicide] has ever been taken up as an option, however, the black knight has a tendency to remain in play.”
– Kay Redfield Jamison“If I were to wish for anything, I should not wish for wealth and power, but for the passionate sense of the potential, for the eye which, ever young and ardent, sees the possible. Pleasure disappoints, possibility never. And what wine is so sparkling, what so fragrant, what so intoxicating, as possibility!”
– Soren Kierkegaard







Leave A Comment